Introduction
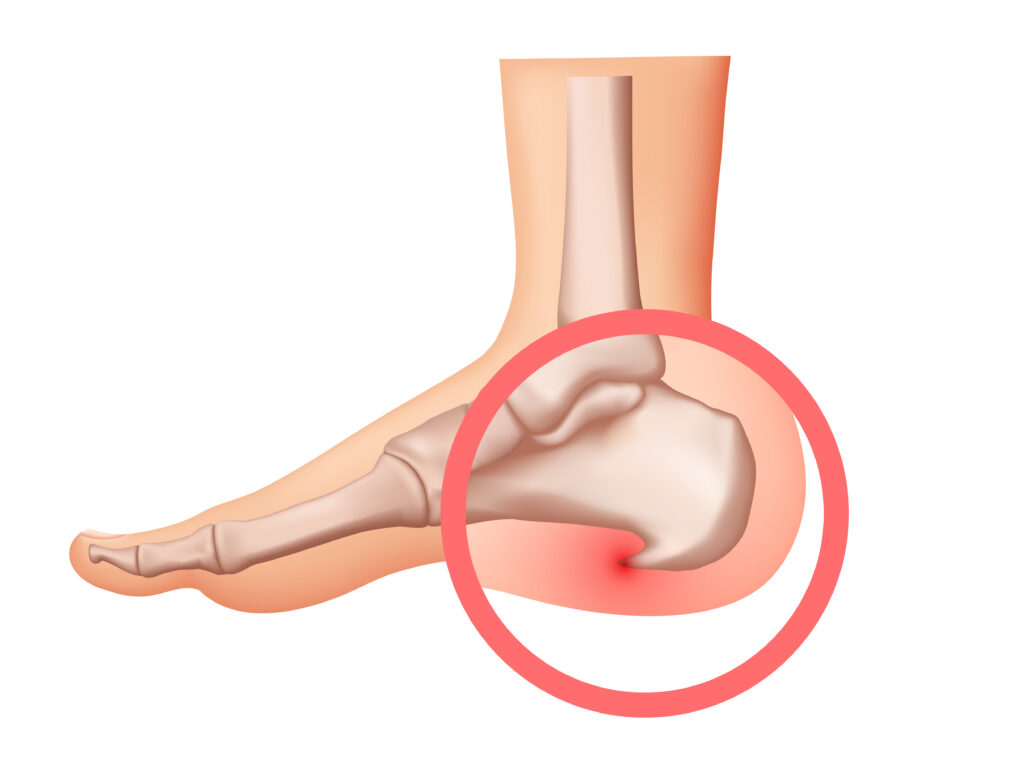
Plantar fasciitis is a common cause of heel pain. Many people feel sharp pain in their heel, especially in the morning. This condition happens when the thick band of tissue on the bottom of your foot becomes inflamed. As a result, walking or standing can be difficult. If you are looking for heel pain relief or want to know about plantar fasciitis treatment options, this guide will help. Understanding foot inflammation causes can also help you prevent future problems.
What is Plantar Fasciitis?
Plantar fasciitis is the swelling of the plantar fascia. The plantar fascia is a strong band of tissue that runs along the bottom of your foot. It connects your heel bone to your toes. When this tissue becomes irritated, it can cause pain and stiffness. Usually, the pain is worst when you take your first steps in the morning. Over time, the pain may get better as you move around, but it can return after long periods of standing or sitting.
Common Symptoms of Plantar Fasciitis
People with plantar fasciitis often notice certain signs. These symptoms can make daily activities hard. However, knowing what to look for can help you seek help sooner.
Sometimes, the pain may feel like a dull ache. But, for many, it can be sharp and sudden. If you notice these signs, it is important to pay attention to your feet.
Causes and Risk Factors
There are several reasons why plantar fasciitis can develop. Often, the cause is repeated stress on the foot. However, some people are more at risk than others.
In addition, tight calf muscles can increase your risk. If you have any of these risk factors, you may want to take extra care of your feet.
How Plantar Fasciitis is Diagnosed
Doctors can usually diagnose plantar fasciitis based on your symptoms and a physical exam. First, your doctor will ask about your pain and when it started. Next, they will check your foot for tenderness and swelling. Sometimes, they may ask you to move your foot in different ways. In rare cases, your doctor may order an X-ray or MRI. These tests help rule out other causes of heel pain, such as fractures or nerve problems. According to the CDC and Mayo Clinic, most cases do not need special tests.
Treatment Options for Plantar Fasciitis
There are many ways to treat plantar fasciitis. Most people get better with simple steps at home. However, some may need more advanced care.
For most people, these steps work well. But, if pain lasts for more than six months, surgery may be an option. Surgery is rare and only used when other treatments fail. Always talk to your doctor before starting any new treatment.
Lifestyle Tips and Prevention
Making small changes can help prevent plantar fasciitis or stop it from coming back. Here are some helpful tips:
By following these steps, you can lower your risk of foot pain. In addition, staying active and healthy supports your overall well-being.
When to See a Doctor
If your heel pain does not improve after a few weeks of home care, it is time to see a doctor. Also, if the pain is severe or you have trouble walking, seek help right away. Sometimes, other conditions can cause similar symptoms. Therefore, a doctor can make sure you get the right diagnosis and treatment. According to the CDC, early care can prevent long-term problems.
If you experience persistent heel pain, consult a healthcare specialist for personalized advice.